Heart Health on Evidation
In collaboration with the American College of Cardiology (ACC), Evidation has launched a nationwide initiative focusing on the lived experience of individuals with heart failure beyond the clinic walls, to understand their particular needs and sources of value which could improve engagement and outcomes.
Over 1000 people with heart failure and other chronic conditions (as of April 2021) from across 48 states and the District of Columbia have agreed to participate, recruited in less than 1 month from Evidation’s app.
Person-Generated Health Data
PGHD allows us to understand the heart failure lived experience outside the clinic for a wider population, and allows individuals to tell their own story.
Engagement
Through PGHD, we can identify individuals who could benefit from engagement and nudge them towards evidence supported actions.
Digital Tools
We can identify individuals with heart failure that are not being managed well and engage them via digital tools, ultimately improving health outcomes.
Important Insights: As of November 29, 2021
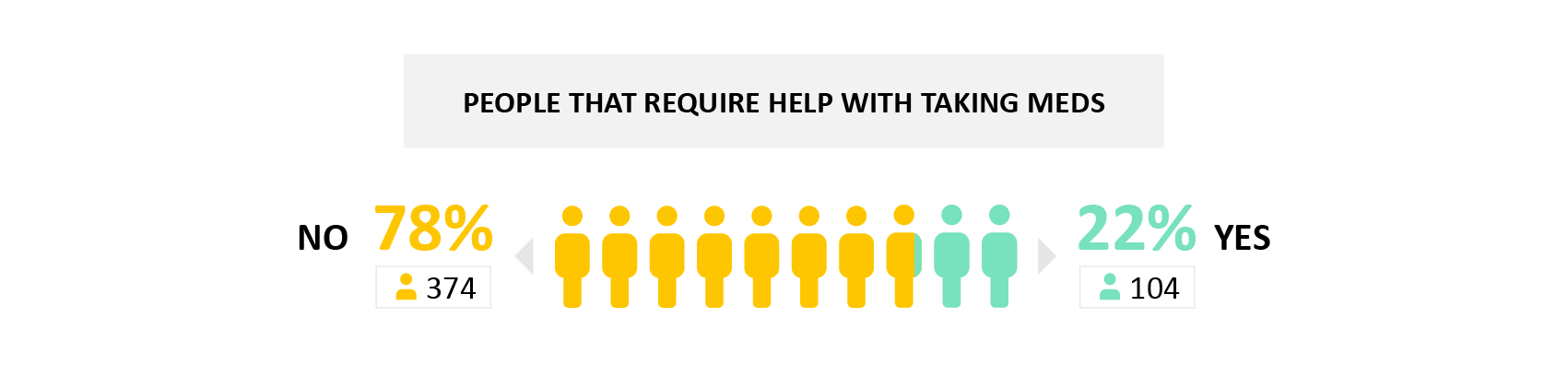
Medication Assistance
22% reported needing help with taking their heart health medications.
- Why it matters: Medication adherence is critical for chronic disease but involves complex behaviors and components including processes and clinical and patient factors. Knowing that a set of patients will require additional help is an important first step to ensuring better ongoing care and management.
Medication Assistance: Demographics
People that require help with medication tend to be relatively young, with lower educational levels and having either multiple or no insurance.
- Why it matters: Understanding which populations require more support with medications can allow for more tailored support and drive greater medication adherence.

Medication Assistance: Symptoms
People that require medication assistance tend to report a worsening of symptoms and more frequent personal care limitations.
- Why it matters: Living with heart failure requires both the knowledge and ability to coordinate potentially multiple medications and lifestyle changes in order to improve symptoms and improve quality of life. We show that there exists a group of patients with heart failure who require help with medications and other aspects of their day-to-day personal care. These individuals may also be more at risk for worsening of symptoms over time (or since last hospitalization). This indicates that targeted interventions and programs that provide social and real-world support may be needed for these vulnerable patients so that they can maintain adherence to their treatments.
.png?width=1701&height=725&name=Figures_Figure%203%20(1).png)
Missing Medication: Changes and Forgetfulness
People that require medication assistance change medication more often, but also tend to not take them more often.
- Why it matters: Identifying triggers for needing assistance - like a recent medication change, or forgetting to take doses - can allow for the development of tools and support mechanisms (like reminders, tracking apps) to improve the consistency of taking medications.
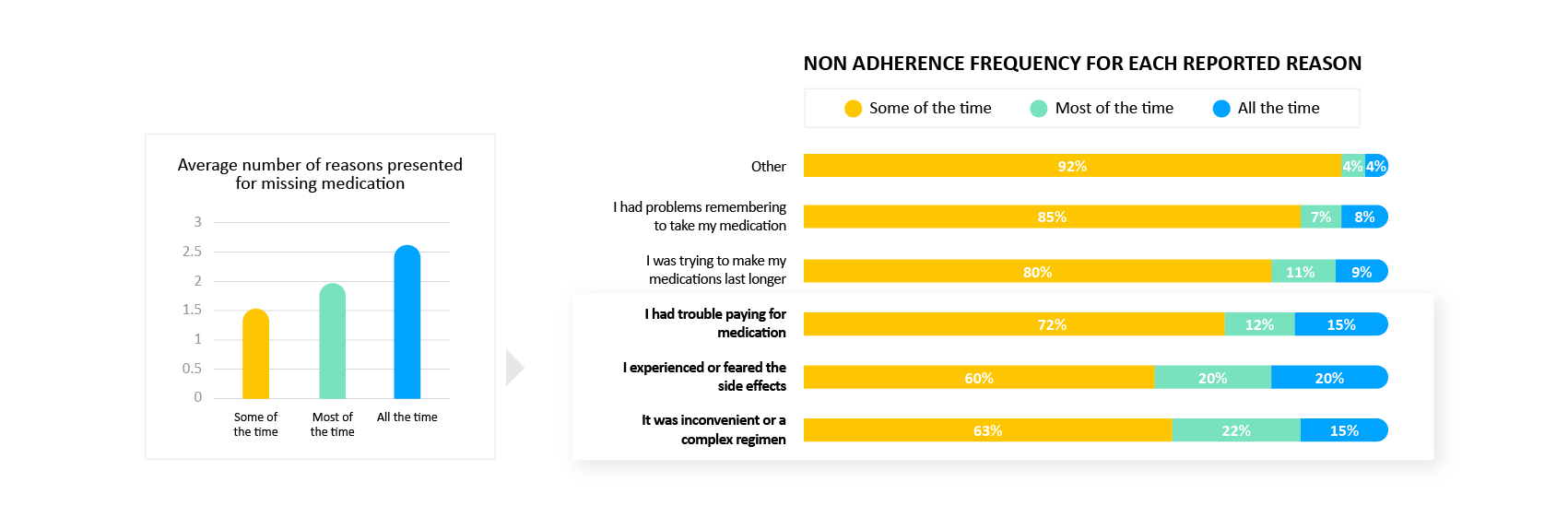
Missing Medication: Reasons
People that miss medications more often also tend to report more reasons for missing it. This includes side effects, complexity and financial constraints.
- Why it matters: A complex set of factors can drive missing medications. Understanding the range of root causes can allow a more comprehensive support strategy tailored to an individual’s specific situation.
Missing Medication: Socioeconomic Status
People that tend to miss medications more often are relatively young, with lower educational degree and have large households
- Why it matters: Various socioeconomic factors and social determinants have been found to be related to medication adherence in those living with heart failure. Of these, we find results consistent with the existing literature, namely that those with less education report more issues with remaining adherent to their medication. We also find that younger patients are slightly more likely to report issues with medication adherence. While this may be surprising, much of the literature exploring heart failure and medication adherence tends to focus on older adults, and uses coarse age range buckets (e.g. < 65 vs > 65 years old). Our findings indicate that it may be useful to explore the younger end of the heart failure patient spectrum to better understand and assist this group.

Medication: Smoking Tendencies
People that tend to miss medications more often tend to smoke and use a walking device
- Why it matters: Previous research has indicated that smoking behavior, as well as body mass index (BMI), is associated with low medication adherence trajectories in those with heart failure. Programs should assist in identifying those patients with factors associated with a risk for low medication adherence early, and applying personalized and supportive adherence management strategies and interventions.

Important Insights: As of July 22, 2021
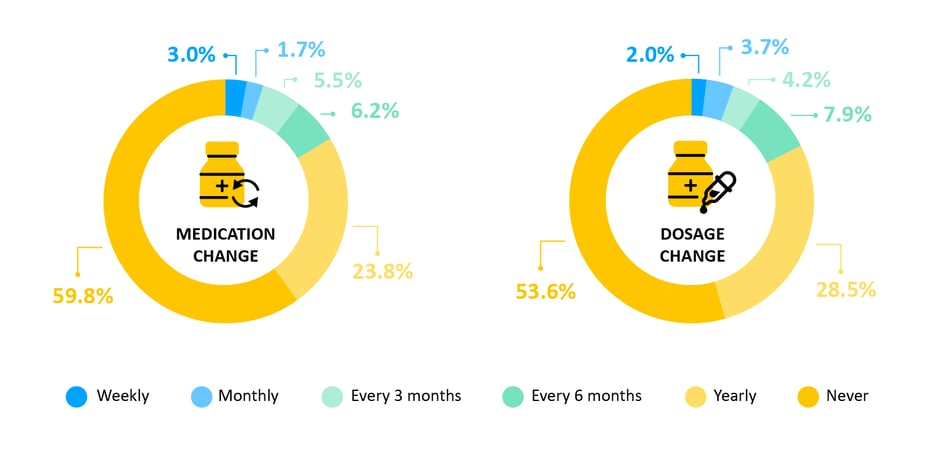
Medication Change
While more than half of the patients actively taking medication to manage their heart health report having never changed either the medications or the dosages they are on, we see a huge range in the rates with which the others report that their medication and the dosages of their medications are changed.
- Why it matters: Getting on the right medication is really important for long-term management of heart failure and a patient’s quality of life. We tend to see a wide variation in medication change due to different causes such as limited access to medication, knowledge etc. Unfortunately, medications are not one size fits all and there is no one correct medication or dosage for all patients. This means that regularly monitoring patients and adjusting their medications and dosages is a key part of successful long-term management of heart failure.
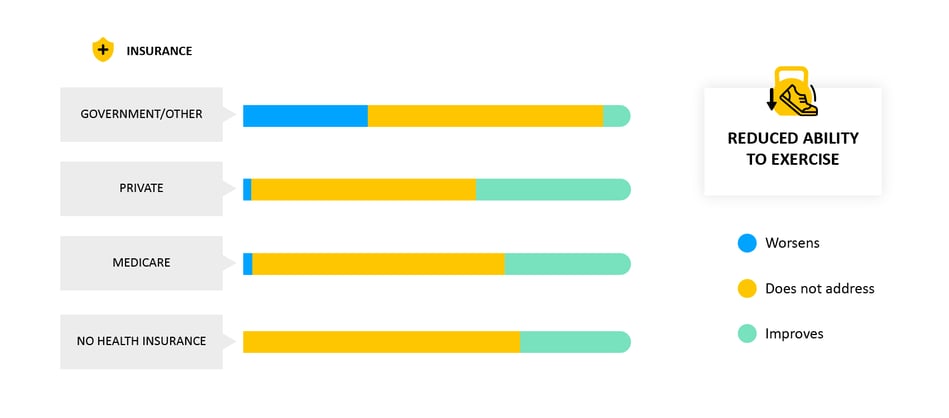
Symptoms by Medication Change
We asked patients how their symptoms changed after their most recent medication change. We saw that a change usually had no effect on specific symptoms, but often helped. However, patients on government (Medicaid, TRICARE or military) insurance, the opposite trend was seen - heart failure often results in a reduced ability to exercise, and patients on government insurance told us that their new medications often made this worse.
- Why it matters: When medications are changed, it is important to monitor if and how symptoms change afterwards. Having a direct connection to patients can help record what symptoms patients are experiencing and facilitate feedback to their doctor, helping them get on the right medications for them.
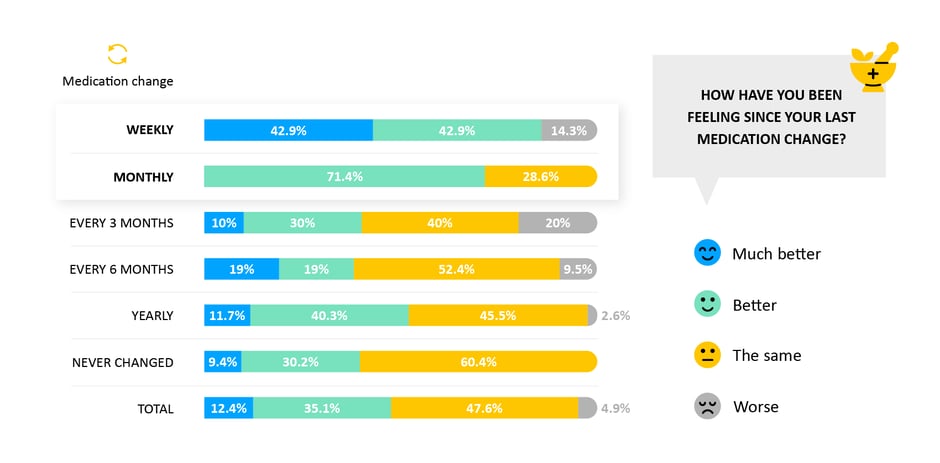
Medication Impact on Well-Being
We asked patients how they were feeling overall since their last medication change. We saw that patients who changed their medications more often (e.g. monthly) felt better overall.
- Why it matters: Finding the right medications for each patient is a big challenge in heart failure, so being in regular contact with your doctor, and regularly updating your medications is a key part of the journey towards well managed heart failure. A direct connection to patients can help track how patients are feeling and nudge them towards healthy choices.
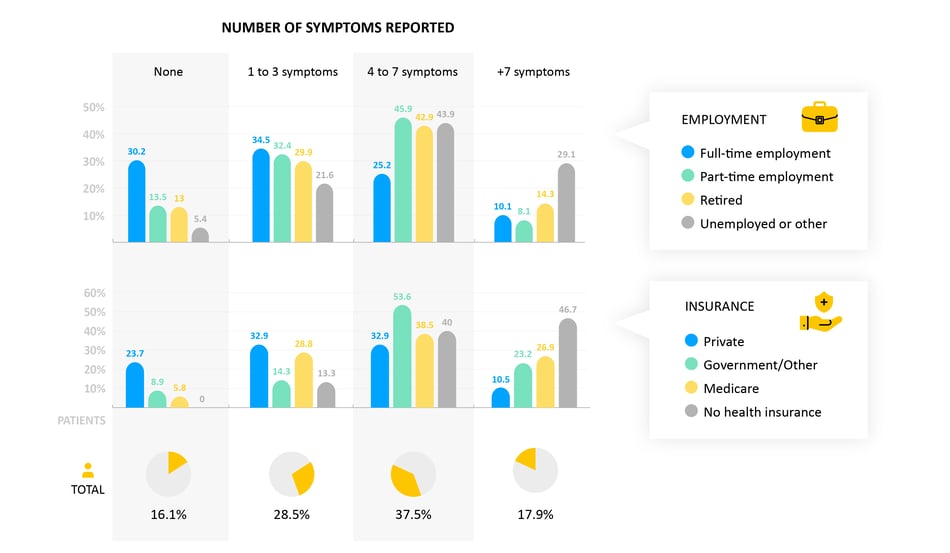
Symptoms by Socioeconomic Status
We see that socioeconomics (for example employment status or the type of insurance someone is on) associates strongly with the number of symptoms an individual reports.
- Why it matters: Socioeconomics have a big influence on access to care and on outcomes in heart failure. Meeting patients where they are, to help them manage their health, is a key part to overcoming these disparities.
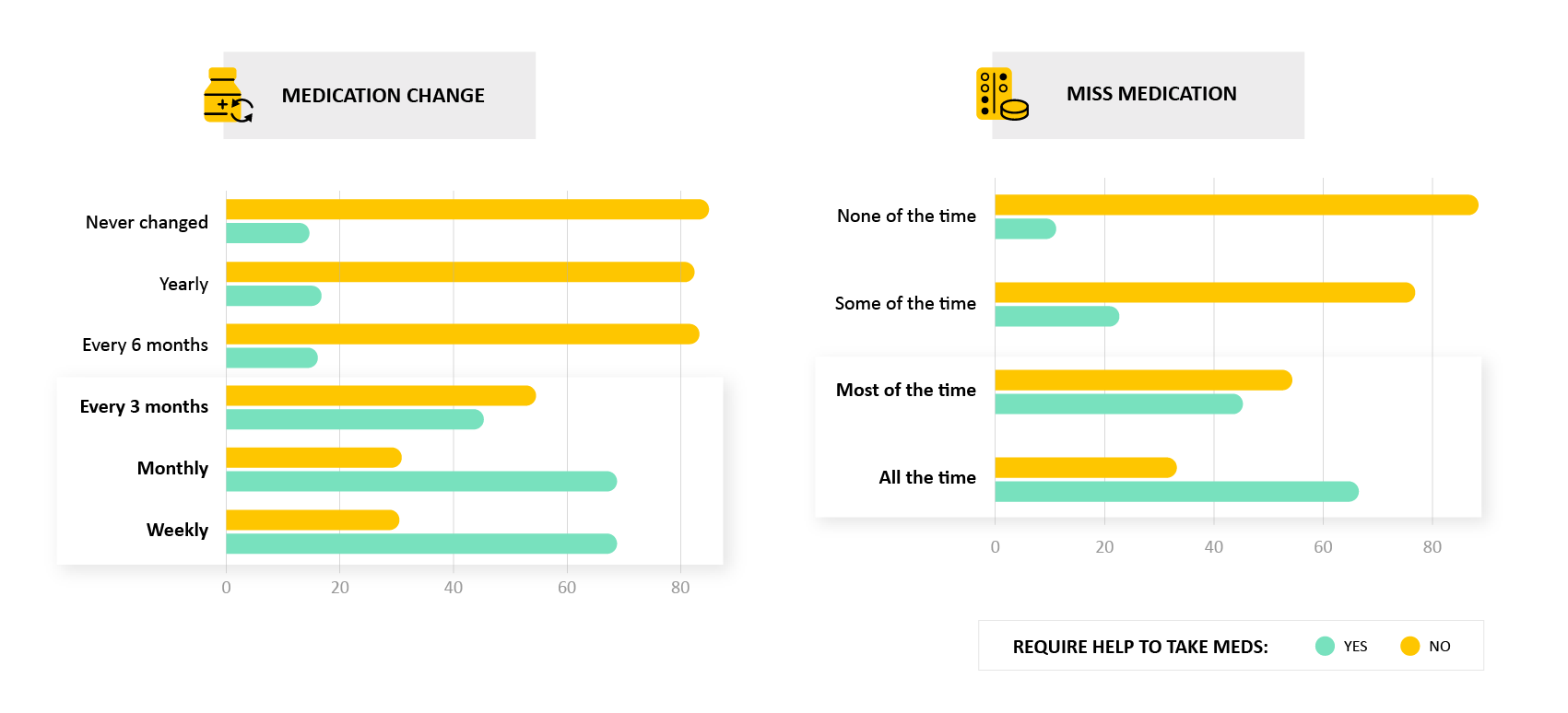
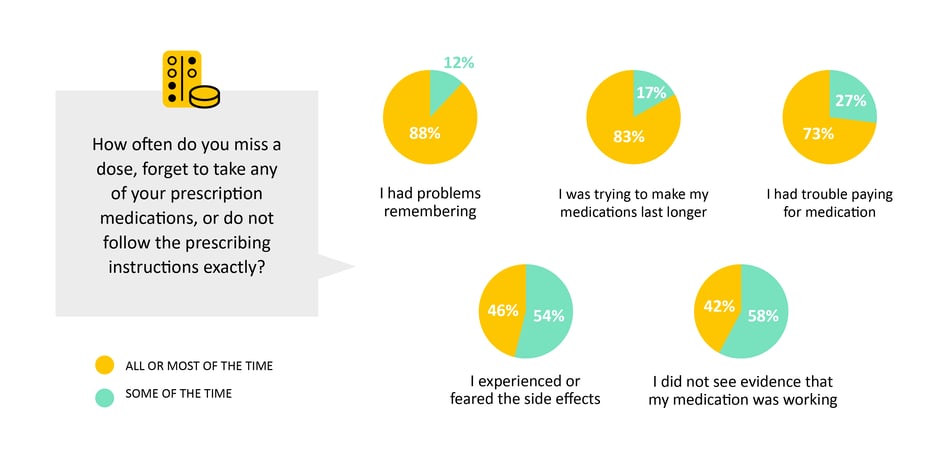
Missing a Dose of Medication
We asked patients how often they miss a dose of their medications and why. The most common reason for occasionally missing a dose was simply because they forgot, but we also saw that many patients reported having trouble paying for medications or tried to stretch their medications to limit costs. In addition, patients who avoided or stopped taking their medications reported having concerns about the medication, experienced side-effects or believed the medications did not work on them.
- Why it matters: Non-adherence can have serious consequences. In the simplest cases, patients need help managing their medications, but we also need to help patients work with their care team to transition to the best medications for them so that they feel the benefit of taking them.
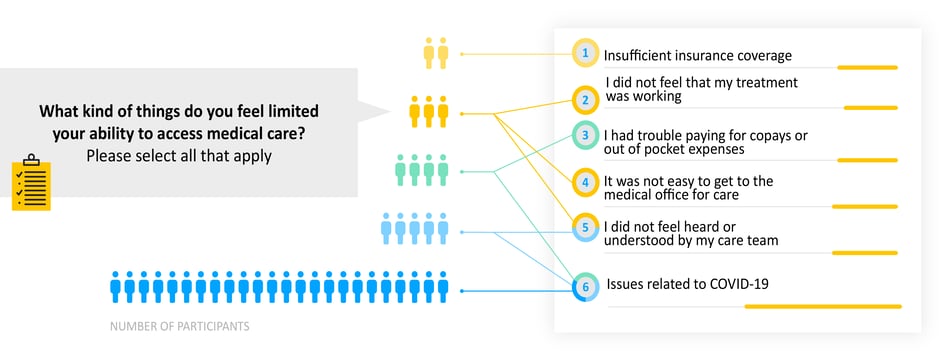
Access to Healthcare
Many heart failure patients experience limitations in access to healthcare. Patients told us that the number one reason for experiencing limitations has been the pandemic.
- Why it matters: The pandemic has affected us all in so many ways, but for heart failure patients and others with chronic conditions, good access to healthcare has been heavily impacted. Enabling patients to access healthcare through other channels will help alleviate this disparity.
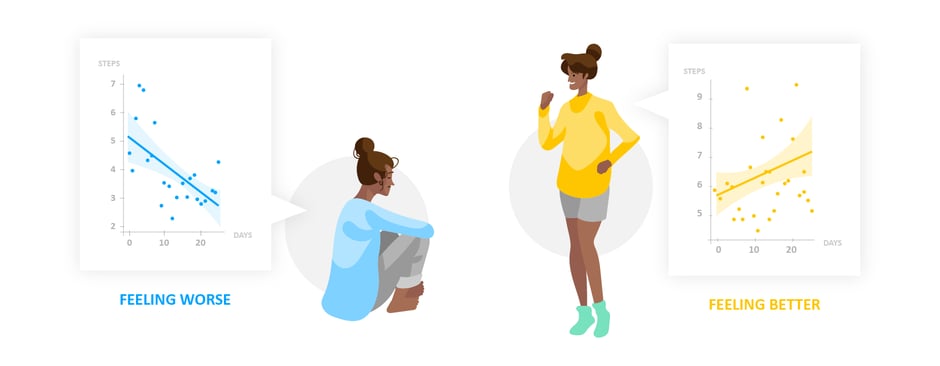
Trends in Activity
We compared self-reported trends in overall health with objective behavioral data collected from consumer-grade wearables. It was found that people who reported feeling better tend to have increased their activity levels over the preceding few months.
- Why it matters: When someone is on a good track, we need objective ways to reinforce that trend. Equally, if someone is off track, we need triggers to reach out to them. This objective Person-Generated Health Data (PGHD) from consumer-grade wearables, enables us to do that.
Important Insights: As of May 25, 2021
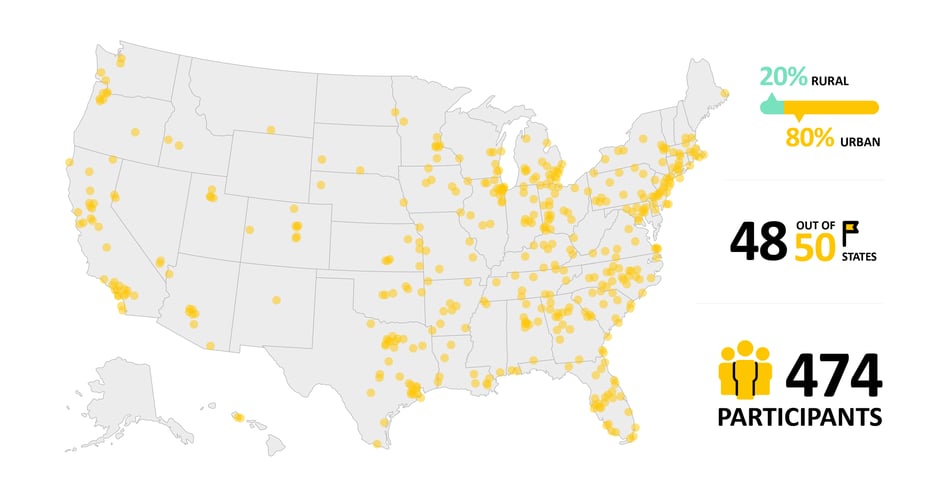
Geographic Reach
474 heart failure participants from across the United States joined the study, representing 48/50 states and a 80:20 mix of urban and rural.
- Why it matters: Inequalities in access and treatment play a large role in Heart Failure outcomes, it is critical to meet patients where they are, both in their journey and also physically.
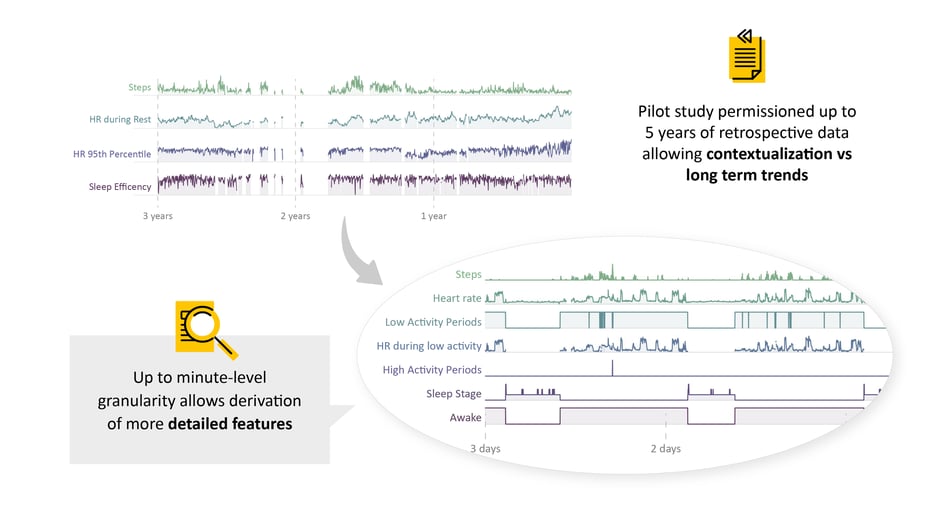
Behaviorgram
Participants shared up to 5 years of retrospective wearable data, in many cases covering their entire heart failure journey: pre-diagnosis, diagnosis, hospitalizations and medication changes, as well as current symptoms and trajectories.
- Why it matters: Participants are enabling us to understand their entire journey and study the impact of heart failure on their behavior and outcomes over long periods of time. This helps us identify individual personas and trajectories, and derive personalized insights which help that individual engage with their own health.
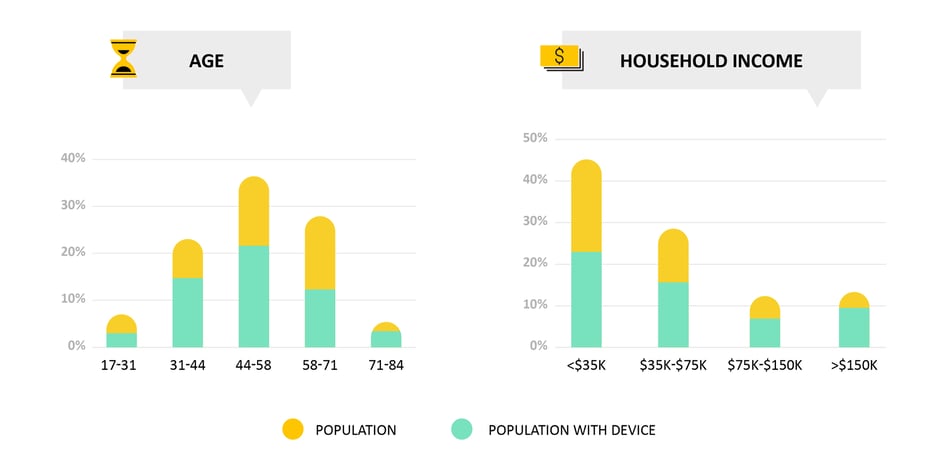
Device Usage
We observe high levels of device usage across demographic, socio-economic and ethnic groups.
- Why it matters: Low-burden and highly popular mobile technologies enable all patients to have their voice heard.
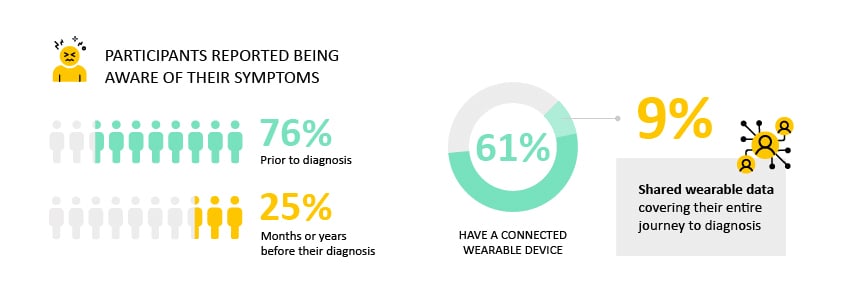
Diagnoses
76% of participants reported being aware of their symptoms prior to diagnosis, and 25% for months or years before their diagnosis. 61% participants have a connected wearable device, of which 9% participants shared dense (no more than 4 consecutive missing days, no more than 15 days missing in a month) wearable data covering their entire journey all the way to diagnosis.
- Why it matters: Diagnosis of heart failure remains a challenge, these data will help us to identify at-risk patients.
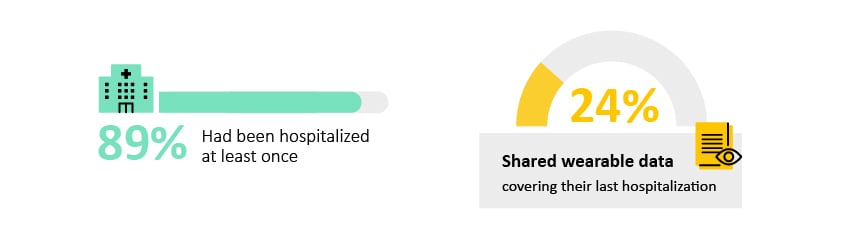
Hospitalizations
89% of participants had been hospitalized at least once, and 24% participants shared dense (no more than 4 consecutive missing days, no more than 15 days missing in a month) wearable data covering their most recent hospitalization.
- Why it matters: Hospitalization is the major driver of costs associated with heart failure in the United States. This data will enable us to better understand behaviors and identify patients who are likely to be readmitted.
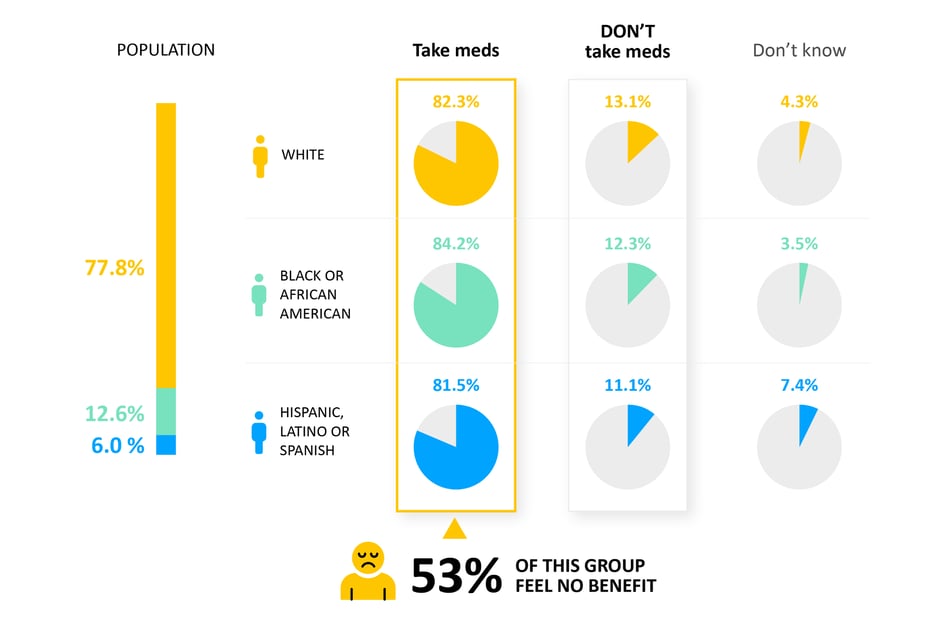
Medication Change
11-13% report not regularly taking any medications for their heart failure, and of those that are, 53% participants reported feeling no change or worsening symptoms since last medication change.
- Why it matters: The majority of patients are not receiving guideline-directed therapy. This data will help us identify sub-optimally treated individuals.
Would you like to partner with Evidation?
We use cookies for data analytics, which helps us understand how you use our site and improve your experience. To learn more about the cookies we use and how to change your cookie settings, click here.
